Both leaders found many common views about ultrasound imaging- including the status of the current global state of health and the future of non-invasive diagnostics. Since the early 70's, Dr. Bard paved his avenue with exploratory research, committing to the movement by collaborating with global colleagues. He based a practice on pushing the boundaries of ultrasound in areas like cancer, chronic disorders and some of the most challenging pathologies. Dr. Ramos, a family physician took point of care ultrasound onto the international stage (with the support of the W.H.O.) by bringing education and access to POCUS in resource-limited settings throughout underserved areas of the world. Together, their mission to drive the ultrasound movement, its benefits to the community and its appeal to just about ANY economic platform rang louder than ever, with both crusaders on the mic.
 |
| Courtesy of GUSI- Global Ultrasound Institute |
-------------------------------------------------------------------------------------------------------------------------
WHO IS DR. MENA RAMOS
While working in rural and underserved regions—across Latin America, sub-Saharan Africa, and Southeast Asia—Dr. Ramos encountered countless barriers to care. Imaging, often taken for granted in developed nations, was a rare luxury in these settings. Something as simple as diagnosing an ectopic pregnancy, a pleural effusion, or a gallbladder issue became life-threatening without the appropriate tools. For her, this wasn’t just a clinical gap—it was a systemic failure.
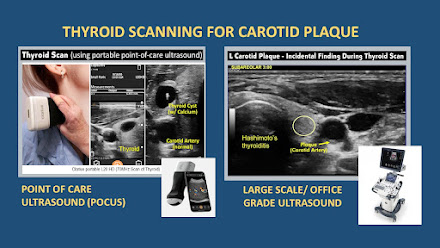
What struck her most profoundly was how POCUS could level the playing field. Unlike MRI or CT, ultrasound required no massive infrastructure, and with handheld devices becoming increasingly affordable and easy to use, the technology held promise for revolutionizing diagnostic care in low-resource settings. It was this potential—of democratizing access to accurate, fast, and safe imaging—that turned her professional interest into a mission.
Dr. Ramos became an active proponent of teaching POCUS as a skill, not just a tool. She emphasized the importance of building local capacity, rather than creating dependency on external aid. In the communities she served, she often ran hands-on workshops for local clinicians, nurses, and midwives—many of whom had never seen an ultrasound machine before. By training them directly, she empowered them to perform high-stakes assessments in real time, reducing diagnostic delays and unnecessary referrals.Beyond the clinical benefits, she saw POCUS as a form of health equity. It closed the gap between urban hospitals and rural clinics. It allowed maternal care in villages without obstetricians. It supported trauma triage in conflict zones and disaster relief areas. In her view, ultrasound was more than technology—it was a translator, a bridge, a voice for patients whose symptoms might otherwise go unheard.
Her work has also involved collaborating with global health organizations and academic institutions to expand ultrasound training curricula. She has spoken on international panels and participated in multi-center research focused on improving ultrasound accessibility. Dr. Ramos continues to advocate for the integration of POCUS into primary care, emergency response, and even community health worker protocols—pushing for a broader redefinition of who gets to use advanced diagnostic tools.In her current practice, Dr. Ramos blends clinical care with outreach, mentorship, and education. She champions interdisciplinary efforts to scale up training and encourages medical students to think beyond hospital walls. "POCUS reminds us that healthcare doesn't have to be centralized to be effective," she says. "It can—and should—travel to where it's needed most."
Dr. Ramos’s story is one of innovation rooted in empathy, and of science in service to equity. Through her work, she’s helping to shape a future where no patient is invisible due to their location, and where frontline care is empowered by information, not restricted by geography.








No comments:
Post a Comment